What is Leukopenia and Agranulocytosis?
The proportion of leukopenic conditions among other diseases of the blood system is quite large. Statistics show an increase in the number of patients with severe leukopenia in recent years. Often, the development of this pathology is in a certain connection with the use of new bacteriostatic agents in medical practice, with exposure to ionizing radiation, as well as with an increase in episodes of allergic diseases. In assessing leukopenic conditions, the doctor should avoid two opposite trends: in some cases, due attention to leukopenia, which is the beginning of a severe pathology of the blood system, is not taken and necessary preventive and curative measures are not taken, in others, any reduction in the number of leukocytes is regarded as a symptom of a severe pathology with unreasonable the use of potent leukopoietic agents (agents that increase the intensity of the formation of these blood cells). Therefore, in order to properly assess the value of “individual” leukopenia, it is necessary, if possible, to find out its causes and development mechanism, since only such a solution of the issue ensures the success of therapeutic and preventive measures in each individual case. Leukopenias are often combined with a significant decrease in the number of neutrophils in the peripheral blood; therefore, they are essentially neutropenia or granulocytopenia (respectively, a decrease in the number of neutrophils and granulocytes).
The causes of granulocytopenia, with all their diversity, are divided into exogenous (acting from the outside), endogenous (arising in the organism itself) and hereditary. The first group of factors includes some substances that have a toxic effect, such as benzene, toluene, arsenic, mercury; some medications; radiation; infectious diseases.
Endogenous causes of neutropenia may be a violation of the endocrine regulation of granulocytopoiesis, i.e. the formation of granulocytes (thyrotoxicosis, adrenal insufficiency, impaired pituitary function), increased spleen function, allergic conditions.
The listed leukopenias belong to the functional group. But leukopenia and neutropenia can be a manifestation of impaired bone marrow hematopoiesis in systemic blood pathology: acute leukemia, hypo– and aplastic states. In some cases, it is not possible to identify a causal factor leading to the development of granulocytopenia. Recently, these forms are becoming less.
In recent years, a special group of hereditary neutropenia (permanent and periodic neutropenia) has been distinguished. In addition, leukopenia may be symptomatic in the form of a non-permanent hematological sign in some diseases.
Moderate asymptomatic leukopenia without any clinical manifestations are detected by chance, are one of the minor and optional symptoms of various diseases. Characterized by a moderate decrease in the number of leukocytes (up to 3.0-4.0 H 109 / l) and unsharp granulocytopenia (40-60% of the total number of neutrophils). The functional properties of leukocytes are not changed. Myelopoiesis is not broken. Bone marrow is normal. There are also no changes in the formation of red blood cells and platelets. Such leuko- and neutropenias are most often purely symptomatic in nature, accompanying a number of diseases not related to the blood system (thyrotoxicosis, gastritis, enterocolitis, cholecystitis, and many others).
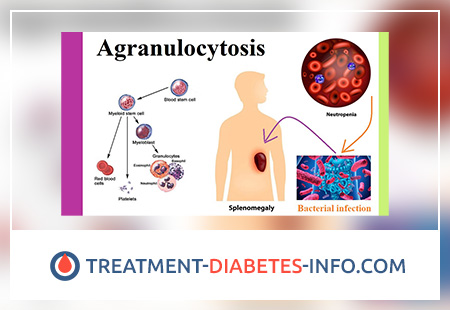
Severe leukopenia is usually accompanied by a sharp decrease in the number of neutrophils in the peripheral blood and is called agranulocytosis.
It is very important to determine when it is safe to talk about leukopenia. In the existing manuals on hematology and physiology, as well as in health care centers, the normal content of leukocytes is indicated, which is 6.08.0 × 109 / l, and the physician proceeds from these figures when assessing pathological changes.
In recent years, the attention of hematologists of all countries has been attracted by the fact that in the absence of any pathology, completely healthy people show a reduced number of leukocytes (from 4.0 to 2.0-2.5 × 109 / l) with moderate neutropenia and relative lymphocytosis. in leukocyte formula. In this regard, mass studies of the peripheral blood of healthy individuals were carried out, which made it possible to expand the narrowed rate of white blood cell count from 4.0 to 9.0 × 109 / l. In everyday practice, the content of leukocytes less than 4.0 H 109 / l can be regarded as leukopenia, and more than 9.0 H 109 / l – as leukocytosis. The limits of normal fluctuations in the percentage of stab neutrophils to 7%, monocytes to 10%, lymphocytes from 19 to 40%, and eosinophils to 5% are also expanded. Therefore, those cases where there are low numbers of leukocytes (up to 4.0–3.0 × 109 / l) in which a thorough clinical and hematological examination and follow-up do not reveal any pathology can be regarded as “safe leukopenia”. In the development of such leukopenia, it is primarily the individual constitutional feature of the regulation of blood formation in each person that matters. In such cases, no therapy is required to stimulate bone marrow formation and leukocyte access to the peripheral blood.
Agranulocytosis is based on a clinico-hematological syndrome, characterized by the complete or almost complete disappearance of granulocytes from peripheral blood. Agranulocytosis should be taken as a condition characterized by a decrease in the number of leukocytes to 1 H 109 / l (1000 in 1 mm3) and lower with a decrease in the absolute number of granular leukocytes less than 0.5 H 109 / l (150 in 1 mm 3).
Pathogenesis during Leukopenia and Agranulocytosis
Agranulocytosis is divided into two main forms: myelotoxic and immune.
The cause of myelotoxic agranulocytosis can be cytostatic factors of any nature – chemotherapy drugs (mercaptopurine, methotrexate, cyclophosphamide, myelobromol, Tio-Tef), ionizing radiation, as well as some drugs that are not used as chemotherapy drugs with a cytostatic target, but also have a snore, and you can also have other drugs, you can use them, you can also have them. chlorpromazine).
The mechanism of myelotoxic agran – leocytosis is due to the suppression by cytotoxic factors of the precursor cell myelopoiesis or the polypotent stem cell.
A similar hematological picture is observed in acute leukemia, in the terminal stage of chronic myeloid leukemia, bone marrow metastases, cancer and sarcoma, which also cause depression and normal hematopoiesis, resulting in agranulocytosis.
Unlike myelotoxic, immune agranulocytosis is caused not by stopping the production of neutrophils, but by their death in the blood and bone marrow, sometimes up to the precursors of granulocyte series due to the appearance of anti-granulocyte antibodies (antibodies against granulocytes). There are hapten immune agranulocytosis and autoimmune. The first occurs under the influence of drugs that are haptens (incomplete antigens), which include aminodopyrin, analgin, butadione, sulfonamides, methylthiouracil, mercury, diuretic, antituberculosis drugs – PASK, ftivazid, tubazid. The combination of antibodies with antigens, which are fixed on the surface of leukocytes, is accompanied by agglutination (“gluing”) and cell death. In autoimmune agranulocytosis, anti-leukocyte antibodies (antibodies against leukocytes) result from a perverse reaction of the immune system with the formation of autoantibodies to leukocytes with an unchanged antigenic structure. Often observed with large collagenosis (systemic lupus erythematosus, rheumatoid arthritis).
In the development of myelotoxic agranulocytosis, the decisive role is played by the magnitude of the damaging effect — doses of the drug, ionizing radiation, the degree of suppressive effect of atypical cells during tumor processes. In immune agranulocytosis, the dose of the causative factor is not crucial, since the most important role in this case belongs to the individual sensitivity of the organism.
Symptoms of Leukopenia and Agranulocytosis
There are differences in the clinical manifestations of myelotoxic and immune agranulocytosis. Immune agranulocytosis, associated with the medication of the hapten row, often develops acutely, with a rapid increase in symptoms. Shortly after taking the medication, granulocytopenia or agranulocytosis, high fever and rapid adherence of infectious complications develop (angina, stomatitis, nasopharyngeal candidiasis, and sometimes esophageal mucosa). Septic complications are the main danger to the life of the patient. Necrotic tonsillitis is a classic manifestation of agranulocytosis. On the tonsils found a dirty gray patina, then – necrosis and ulcers. Necrotization captures the tongue, soft and hard palate; bleeding often occurs. However, necrosis can also be localized in the intestine, flowing with a typhoid-like pattern, in the esophagus, bladder, and female genitals. In the lungs pneumonia often develops, which occurs atypically, often leads to the formation of an abscess, gangrene. The liver can be moderately enlarged, the size of the spleen, as a rule, is not changed. Jaundice is quite rare; in the urine – moderate albuminuria (protein in the urine) associated with a septic condition.
In immune blood agranulocytosis, leukopenia, absolute agranulocytosis, is noted. The number of erythrocytes, reticulocytes, platelets is not changed. Hemorrhagic syndrome is not pronounced. The bone marrow is not devastated, there is a slight decrease in its cellular composition. Only when agranulocytosis aggravates aggravation of the bone marrow.
Myelotoxic agranulocytosis has features of the clinical and hematological picture, which is determined by the specifics of its development – high sensitivity to damage to stem and ripening bone marrow cells and very low sensitivity of mature elements. It starts suddenly. Without any subjective signs of the disease in the blood decreases the content of leukocytes and, as a rule, reticulocytes and platelets. The first external signs of the disease: fever, stomatitis, “agranulocytic sore throat”, hemorrhagic syndrome — are detected against the background of profound changes in peripheral blood and a sharp decrease in the bone marrow cellularity.
At the same time, damage to the mucous membrane of the oropharynx and the gastrointestinal tract with the development of necrotic enteropathy is one of the most persistent signs of myelotoxic agranulocytosis, which has a dual origin.
Other infectious complications of agranulocytosis also include sepsis (often staphylococcal), mediastinitis (mediastinal inflammation), and pneumonia. In this case, pneumonia occurs against the background of scarce physical and radiological data.
Diagnosis of Leukopenia and Agranulocytosis
The diagnosis of agranulocytosis should be necessarily differentiated from acute leukemia (its leukopenic form).
Diagnostic errors are possible in both directions, most often it concerns morphological errors, when a significant percentage of lymphoblasts are mistaken for lymphocytes, since both of them have some similarities. In some cases, possible “agranulocyte start” of acute leukemia, which at the beginning of the disease mistakenly qualifies as agranulocytosis. Later, the typical leukemic stage of acute leukemia develops. Unlike aplastic anemia, there is no anemic and thrombocytopenic syndrome in agranulocytosis.
The prognosis for plastic (functional) forms of agranulocytosis is favorable, within 2-3 weeks clinical recovery and complete repair (recovery) of the blood occurs. In aplastic forms, the prognosis is more serious, but with timely and reasonable therapy, recovery is possible.
A sign of incipient hematopoietic recovery in patients with agranulocytosis is monocytosis (an increase in the number of monocytes) with the presence of their precursors in the blood.
Treatment of Leukopenia and Agranulocytosis
The main role in the fight against cytopenic conditions belongs to prevention. Given the pronounced effects of radiant energy derived from benzene, strict measures are needed to protect those who are systematically exposed to these factors. One of such measures is control over their blood composition and timely measures to ensure safety measures. This determines the most effective form of dynamic clinical and hematological monitoring – follow-up observation of all persons with leukopenia, neutropenia and cytopenia.
Not every reduction in the number of leukocytes requires energetic, stimulating the formation of leukocyte therapy. Such therapy is necessary where leukopenia is a consequence of impaired bone marrow function. Therapeutic measures for leukopenia of different origin depend on their severity and clinical manifestations. Currently, the clinic uses a significant amount of drugs that have the ability to stimulate the maturation of granulocytes. These include nucleic acid sodium, pentoxyl, leucogen, and bathilol, which are physiological stimulants of leukopoiesis. However, the therapeutic efficacy of these drugs is justified only with moderate leukopenia, especially medication.
In the treatment tactics of agranulocytosis, it is necessary to exclude cytotoxic drugs, ionizing radiation, and drug haptens. Of particular importance is the creation of aseptic conditions (placement of patients in boxes or isolators with installed bactericidal lamps, ultraviolet irradiation of the chambers), and rehabilitation of the skin and mucous membranes.
Treatment of bacterial complications with antibiotics should be urgent from the first days of diagnosis of agranulocytosis. Wide-spectrum antibiotics are used in large doses (penicillin, ampicillin, ceporin, gentamicin).
In immune agranulocytosis, antibiotic treatment is carried out until leukogram is restored and bacterial complications are eliminated. In order to reduce the degree of granulocytopenia and its duration, it is important to use leukocyte, and to combat thrombocytopenic hemorrhages (mainly in the myelotoxic form of agranulocytosis – cytostatic disease) – and platelet mass. For the prevention and treatment of necrotic enteropathy, suppression of pathogenic intestinal flora with sterilization of the intestine with the help of antibiotics (kanamycin, ristomycin, nystatin), as well as intravenous nutrition of patients is used. In the treatment of immune agranulocytosis, corticosteroid hormones play a major role.
Prednisolone, prednisone, triamoinolone, dexamethasone are used as desensitizing agents that suppress the formation of aggressive antibodies and stimulate the maturation of granulocytes. Restoration of the white sprout of the bone marrow in such cases is fast. With the normalization of the number of leukocytes, usually in 10-14 days, the dose of hormones is reduced by no less than half. Treatment with intermittent hormones continues until full recovery and until the disappearance of autoimmune antibodies. When expressed ulcerative-necrotic manifestations, a certain caution is needed regarding the use of corticosteroids. Steroid hormones are contraindicated in patients with myelotoxic agranulocytosis.
The prognosis for immune agranulocytosis is relatively favorable. Early and proper treatment can lead to recovery. In myelotoxic agranulocytosis, the prognosis depends on the severity of the lesion. The overall mortality in agranulocytosis is about 25%, mainly due to necrotic enteropathy, general sepsis, gangrene, and more often with myelotoxic form.
Persons suffering from agranulocytosis, need dispensary observation. This is especially true for those patients who are discharged from the hospital in a satisfactory condition with a sufficient number of leukocytes (3000–4000), but often with a low content of granulocytes. This indicates insufficient and unstable recovery of blood formation. Periodic hematological monitoring of peripheral blood of patients allows detecting a gradual drop in the number of granulocytes. Prevention is real if there is a known cause for the development of this disease. In particular, the drug that caused agranulocytosis or leukopenia should be completely excluded.